After you have visited a doctor, clinic or hospital or filled a prescription, you will get a statement from Blue Cross and Blue Shield of Texas (BCBSTX) that explains what was covered under your plan. This is called an Explanation of Benefits, or EOB.
Understanding Your Explanation of Benefits
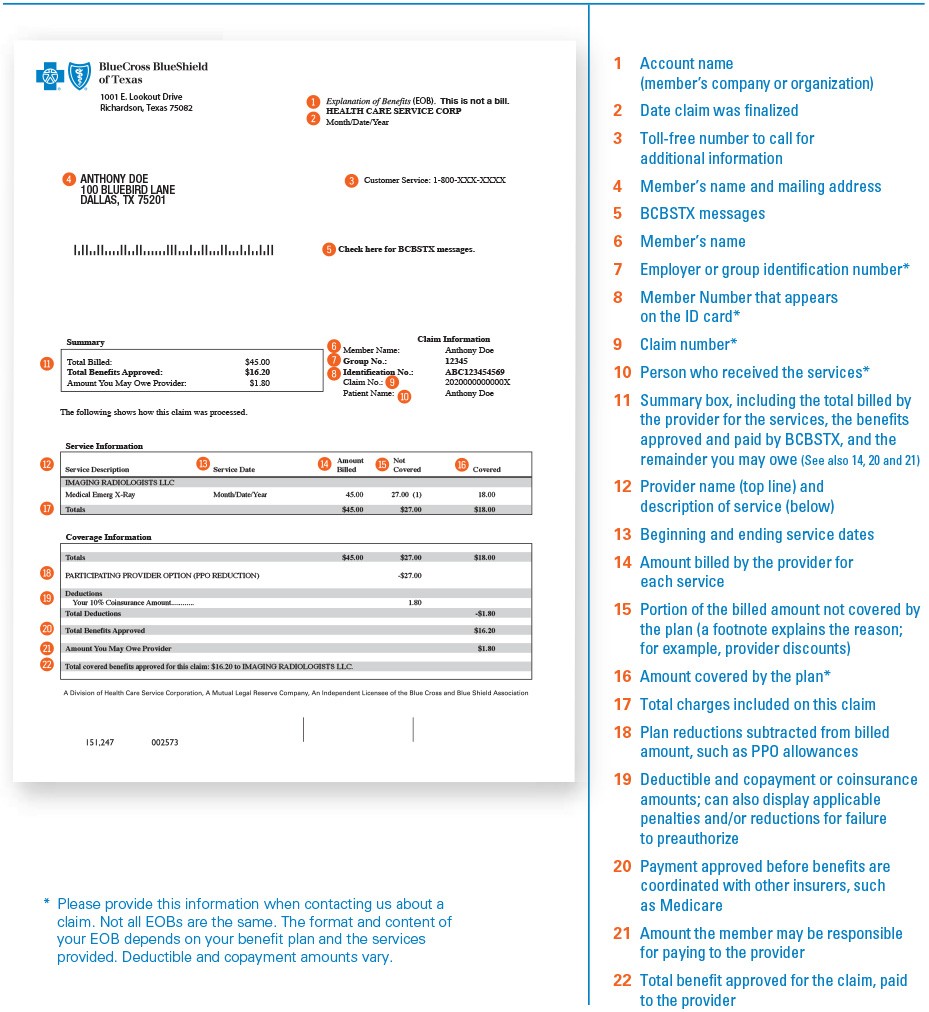
An EOB will have these details:
- The patient and the service provided
- The amount charged by the provider
- The amount of the charges that are covered and not covered under your plan
- The amount paid to your provider
- The amount you're responsible for
The EOB isn't a bill. Anything you owe will be billed from your provider.
You can use your EOB to keep track of how much has been paid toward your annual deductible and out-of-pocket costs.
Your EOB explains your right to appeal if your health plan doesn't cover the provider's claim for care provided.
Sometimes a simple error could cause a claim to not be paid, such as the claim not having the right information. Anytime you have a question about what is on your EOB or how the claim was paid, call Customer Service to talk with a Customer Advocate. We want to make sure you understand your coverage each step of the way.
Your EOB also lists our fraud hotline, a toll-free number to call if you think you are being charged for care you did not receive or by providers you never saw. One of the best ways to stop health care fraud is to catch it at its source.
If you have any questions about an EOB, call us at 888-697-0683 or log into your Blue Access for MembersSM account at bcbstx.com.
Sample EOB
Find
Free In-Person Help
Register to meet one-on-one with our trusted community specialists who can give you the help you need to shop for health insurance.
Downloadable MATERIALS
We offer helpful materials for you to download and keep in case you need more information about the Affordable Care Act (ACA), how to enroll and how to use your health insurance.

